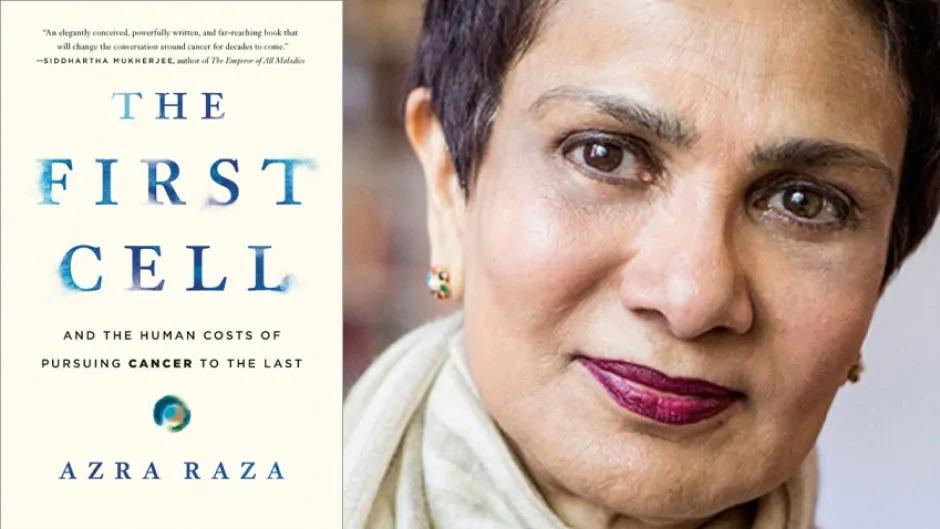
Editor’s Note: This is a letter sent by Dr. Audeh to my sister about her recent book, The First Cell: And the Human Costs of Pursuing Cancer to the Last, and I am publishing it here as a review with his permission.
by M. William Audeh
 May 26, 2020
May 26, 2020
Dear Azra,
I am happy to inform you that upon the end our phone conversation, I opened your book, which had been on my Kindle since its publication, and read it over the long weekend.
My apologies for not having read it earlier, but I had my reasons, which I will explain below. However, let me begin by saying that I thoroughly enjoyed your book, not least because your passionate voice comes through the pages so clearly in your writing. I feel as if I have had the privilege of spending several evenings in your lucid company, discussing these fundamental scientific ideas and sharing the heartfelt sorrows. It is eloquent and wonderfully written; a deeply passionate yet sharply rationale argument and memoir. Congratulations!
I will confess, that although I was quite interested to read your book, having spoken with you about its inception, development and impending publication, I was ultimately hesitant. My reluctance stemmed from two regrettable impulses, about which I am not proud, but will readily admit to you, as a dear friend. One was simple jealousy, that you had written and published a book which expressed your long-held beliefs, and anger at myself, for not having found the time and energy to do so myself. Perhaps reading your book will now inspire me to write my own. The other source of my hesitancy was the belief, not entirely unfounded, that I would find myself disagreeing with you on many points of your discourse and did not want to experience that discomfort in relation to you as a friend and colleague. In truth, I am in agreement with you on so very many aspects of your book, that I feel foolish in having held that concern. However, now that I have read your work, and understand the manner in which you have chosen to lay out your argument, I would like to express my thoughts on what you have written.
You have chosen to illustrate in your book, through poignant patient vignettes, the futility of much of oncology therapy, and the terrible cost of zealously believing we were, and are, on the right track, in our approach to cancer. So many people with early stage cancer have suffered needlessly from excessive or unnecessary therapy, and in advanced cancer, because of the false hope placed in often marginally beneficial and toxic therapies. And you effectively intersperse these patient stories with your clear explanation of the biological underpinnings of cancer, the realities of cancer research, and the clinical hubris which have driven much research and treatment. So much time, and money, and so many precious resources have been spent on misguided research and poorly designed clinical trials. I agree with you that highly engineered biological systems, such as in-vitro cell lines and animal models often bear no useful resemblance to what goes on in the human organism, and the ecosystem of the body, the tissues, and the cellular microenvironment. You do not discount the hopeful findings from well-done research and recent discoveries, but you seek to put them into the appropriate context. I particularly enjoyed the passage, at the end of the book, in which you begin… “I am not saying that animal models should be abandoned. What I am saying is that animal models are misleading…. I am not saying that technologies such as CRISPR are all hype…”.
Azra, I agree with most everything you have written. My differences of opinion may only lie with your conclusions as to where we should go now and in the future. I agree that early detection would be the best solution, were it truly possible in the near term. But I worry that finding a mutated or methylated gene in the circulation which indicates a lung carcinoma will not be helpful if we cannot accurately locate that carcinoma and successfully ablate it. Or be certain that it truly indicates the “line” of malignancy has been crossed somewhere in the epithelium. Or have a ready therapy to reverse the malignant process once we detect it. I would argue that the ability to detect the “first cell” will remain far ahead of the ability to act effectively on its detection for some time. Nevertheless, there are many promising avenues for such technologies, to detect new or recurrent cancer in otherwise healthy people, and I am certainly in favor of devoting many more resources in this arena. However, this does not preclude using what we know now, and could easily know in the near future, for a different approach to treatment and prevention.
I inevitably return to the application of Evolutionary Biology for understanding cancer, to make my points. In one passage in your book, as I interpreted your words, you describe the process by which cancers mutate and change under therapy as the creation of “new cancers”; that a cancer in an individual is actually many cancers. If that is your meaning, then with this I must embrace a different concept. As I interpret evolutionary biology, a “cancer” in an individual is a population of cells. It is an invasive new species, like any other in nature, in an ecosystem to which it is already well-adapted. By virtue of the very origin of its existence, the tolerance of genetic instability, generating mutations which did not lead to apoptosis or senescence, this population is equipped with the ability to mutate quickly and adapt to most any threats to survival. The larger the cancer cell population, the more genetic diversity present to allow survival in the face of selective pressures. Cancer is not many diseases, but a single, unique population of related cells in any one individual, with a phylogeny and lineage which can be traced and understood, and actually predicted. Unfortunately, by the time of clinical diagnosis in many people, the adaptive genomic diversity of the population far exceeds the selective pressures which can be exerted by simple chemotherapy and radiation, or single targeted therapies. The consequence of applying this approach, as many of your clinical vignettes illustrate, is the cruelty of a seeming reprieve, and inevitable resurgence, once the surviving, adapted sub-population expands to become clinically evident and now, resistant to therapy. So, the earlier detection, the better, of course – fewer cells, less adaptive diversity. But to drive this invasive species to extinction requires knowledge of its unique vulnerabilities. We must be able to analyze the genomic anatomy of this species, in order to understand it, and eradicate it. For this, we do need to understand complex pathways and gene expression patterns and functional, molecular analysis, but this challenge is not insurmountable. The pathways are finite, and follow the logic of survival and selection, and can be predicted. There is evolutionary constraint and contingency which limits the pathways taken in the branching phylogeny of a cancer’s family tree. I believe computer learning and AI can help us with such predictions. But we also need effective combination therapies to knock out critical pathways, and block escape pathways, or limit them so that the cancer cell population, if not eradicated, is at least driven into a bottleneck population with reduced numbers and genomic diversity, which the immune system can then handle. In other words, I do believe a treatment strategy based on principles of evolutionary biology aimed at extinction is still possible, if trials and research were directed this way.
However, I believe we should pursue Prevention as well. Although Early Detection, as you promote it, is the logical solution when you believe the development of cancer is inevitable and unpredictable, I do not accept that it is entirely so. I understand that aging and oxidative metabolism and replicative errors happen all the time in the cells of the body. I understand that Vogelstein and colleagues have published data suggesting that most cancer-causing mutations occur by “chance”, and that high penetrance, predisposing germline mutations are rare, concluding that most cancers are therefore “unpreventable”. I strongly disagree with this conclusion, however, because it ignores the impact of variation between individuals, in the form of human genetic and lifestyle diversity.
There exists, in all human populations, great genetic diversity in the form of functional polymorphisms, which are relevant to virtually every step of carcinogenesis. Beginning with Phase I and Phase II metabolism genes, we all process diet and exogenous chemicals differently. We repair DNA damage with varying proficiency. There is additional variation in repair depending on which type of damage it is – oxidative, radiation-related, DNA-adduct related, replication error-related, etc. There is great variation in immune function as well – inflammatory response, immune cell populations, cytokine production, innate immunity, adaptive immunity – which affects whether tissues are damaged by inflammation, and whether an abnormal cell population is recognized or not. And on top of all this genetic variation is layered the individual variation in exposures and lifestyle decisions. So, while individual mutations in cancer-promoting genes may occur by “chance”, the odds of such a mutation occurring may be profoundly affected by our genes and our lifestyles. Some individuals may have higher odds than others of acquiring mutations, due to genetic polymorphisms. Some individuals with low genomic odds may increase their odds of a mutation anyway, by smoking, or living in polluted cities, or causing repetitive rounds of cell division due to hormone stimulation or tissue injury. All of this is measurable. But we do not consider it as a part of routine care. Fair-skinned people are encouraged to use sunscreen, and smoking is generally discouraged, but that is the extent of it! Perhaps we should apply research efforts to reducing mutation rates, by understanding polymorphisms, and gene-environment interactions, and suggesting interventions. “Chance” is the unsatisfying term used when the actual cause of something is unknown, but that does not mean it is unknowable.
Finally, I was struck by your “grains of sand” analogy of cancer, in which the grains fall randomly on a sandpile, until one random grain pushes the mound as you say into a “critical state” from which all cascade downwards. I would argue that if the “grains” are the mutational changes leading to the critical state of “malignancy”, then we may have the ability to control, to some extent, the rate at which new grains are dropping on the sandpile. I am arguing that not all individuals build their sandpiles at the same rate, and we pay little or no attention to how, with knowledge of our own functional genomic diversity, we could slow that rate down. And as we detect early and biologically meaningful mutations on the path to carcinogenesis, we may use that knowledge to intervene further, to actually prevent that last grain of sand from dropping, or that First Cell from emerging.
Thank you for your call on Friday.
It meant a great deal to me. I look forward to continuing our dialogue.
With warm regards,
Bill
***
 Dr. M. William Audeh is a medical oncologist specializing in breast cancer, with over 30 years of experience as a clinician and clinical researcher at the Cedars-Sinai Cancer Center in Los Angeles, where he continues to be a member of the Medical Staff. He has been the Chief Medical Officer for Agendia, a precision oncology company providing genomic profiling of early breast cancer, since 2016.
Dr. M. William Audeh is a medical oncologist specializing in breast cancer, with over 30 years of experience as a clinician and clinical researcher at the Cedars-Sinai Cancer Center in Los Angeles, where he continues to be a member of the Medical Staff. He has been the Chief Medical Officer for Agendia, a precision oncology company providing genomic profiling of early breast cancer, since 2016.
During his years of clinical practice at Cedars-Sinai, Dr. Audeh served as Director of the Cedars-Sinai Cancer Center, Clinical Chief of the Division of Hematology/Oncology, Chair of the Cancer Committee, Medical Director of the Wasserman Breast Cancer Risk Reduction Program and faculty member in the Cedars-Sinai Biomedical PhD program and Breast Surgery and Surgical Oncology Fellowships at Cedars-Sinai. He has had an academic appointment as Associate Clinical Professor of Medicine at the UCLA School of Medicine, where he continues to be a member of the UCLA Evolutionary Medicine Program.
In addition to clinical practice, Dr Audeh regularly lectured on the application of Genomics to Cancer Medicine in the UCLA School of Public Health. From 2009 to 2016, Dr. Audeh was a member of the Full Time Academic Faculty of Cedars-Sinai Medical Center. He has been Principal Investigator on many clinical and translational trials, primarily in breast cancer, and was and was instrumental in the early phase trials with PARP inhibitors. Dr Audeh has authored numerous publications in the field of breast cancer, cancer genomics, and genomically targeted cancer therapy. Has also been a consultant to many of the major pharmaceutical and biotech companies, as well as to all genomic testing companies in breast cancer.
Dr. Audeh received his medical degree from the University of Iowa and an M.S. Degree in Genetics from the University of Minnesota. He completed Residency in Internal Medicine, a year as Chief Medical Resident, as well as a Fellowship in Medical Oncology at Stanford University Medical Center. He is board certified in internal medicine and medical oncology and is a member of the American Society of Clinical Oncology and the American Association of Cancer Research.
