Siddhartha Mukherjee in The New York Times:
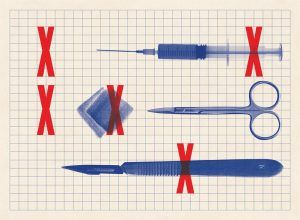 Late last year, I witnessed an extraordinary surgical procedure at the Cleveland Clinic in Ohio. The patient was a middle-aged man who was born with a leaky valve at the root of his aorta, the wide-bored blood vessel that arcs out of the human heart and carries blood to the upper and lower reaches of the body. That faulty valve had been replaced several years ago but wasn’t working properly and was leaking again. To fix the valve, the cardiac surgeon intended to remove the old tissue, resecting the ring-shaped wall of the aorta around it. He would then build a new vessel wall, crafted from the heart-lining of a cow, and stitch a new valve into that freshly built ring of aorta. It was the most exquisite form of human tailoring that I had ever seen. The surgical suite ran with unobstructed, preternatural smoothness. Minutes before the incision was made, the charge nurse called a “time out.” The patient’s identity was confirmed by the name tag on his wrist. The surgeon reviewed the anatomy, while the nurses — six in all — took their positions around the bed and identified themselves by name. A large steel tray, with needles, sponges, gauze and scalpels, was placed in front of the head nurse. Each time a scalpel or sponge was removed from the tray, as I recall, the nurse checked off a box on a list; when it was returned, the box was checked off again. The old tray was not exchanged for a new one, I noted, until every item had been ticked off twice. It was a simple, effective method to stave off a devastating but avoidable human error: leaving a needle or sponge inside a patient’s body.
Late last year, I witnessed an extraordinary surgical procedure at the Cleveland Clinic in Ohio. The patient was a middle-aged man who was born with a leaky valve at the root of his aorta, the wide-bored blood vessel that arcs out of the human heart and carries blood to the upper and lower reaches of the body. That faulty valve had been replaced several years ago but wasn’t working properly and was leaking again. To fix the valve, the cardiac surgeon intended to remove the old tissue, resecting the ring-shaped wall of the aorta around it. He would then build a new vessel wall, crafted from the heart-lining of a cow, and stitch a new valve into that freshly built ring of aorta. It was the most exquisite form of human tailoring that I had ever seen. The surgical suite ran with unobstructed, preternatural smoothness. Minutes before the incision was made, the charge nurse called a “time out.” The patient’s identity was confirmed by the name tag on his wrist. The surgeon reviewed the anatomy, while the nurses — six in all — took their positions around the bed and identified themselves by name. A large steel tray, with needles, sponges, gauze and scalpels, was placed in front of the head nurse. Each time a scalpel or sponge was removed from the tray, as I recall, the nurse checked off a box on a list; when it was returned, the box was checked off again. The old tray was not exchanged for a new one, I noted, until every item had been ticked off twice. It was a simple, effective method to stave off a devastating but avoidable human error: leaving a needle or sponge inside a patient’s body.
In 2007, the surgeon and writer Atul Gawande began a study to determine whether a 19-item “checklist” might reduce human errors during surgery. The items on the list included many of the checks that I had seen in action in the operating room: the verification of a patient’s name and the surgical site before incision; documentation of any previous allergic reactions; confirmation that blood and fluids would be at hand if needed; and, of course, a protocol to account for every needle and tool before and after a surgical procedure. Gawande’s team applied this checklist to eight sites in eight cities across the globe, including hospitals in India, Canada, Tanzania and the United States, and measured the rate of death and complications before and after implementation.
The results were startling: The mortality rate fell to 0.8 percent from 1.5 percent, and surgical complications declined to 7 percent from 11 percent.
More here.
